The healthcare system’s capacity to provide patients more control over their healthcare and higher involvement in the decision-making process has evolved to a great degree. This process is termed ‘patient-centricity’ – and its presence has grown thanks to the spread of the internet and digital technology. From empowering patients by making information accessible, to helping healthcare providers and pharma companies provide patients greater control through connected services, technology has been enabling patient-centricity to grow.
However, despite the developments, we’re still far from achieving a full-fledged patient-centric healthcare system. What’s preventing us from advancing patient centricity? And can market research play a role in advancing our efforts in this field?
The doctor-patient disconnect
Before we could begin to tackle the problem of improving patient centricity, we had to find out where the problem lay. We started by conducting a qualitative survey among a control group of 400 patients and 50 general practitioners (GPs) in the USA and Brazil. We enquired about the problems they faced while interacting with doctors and patients respectively and compiled the observations.
The study provided the following insights on the barriers to patient-centricity (all %’s Brazil & US combined):
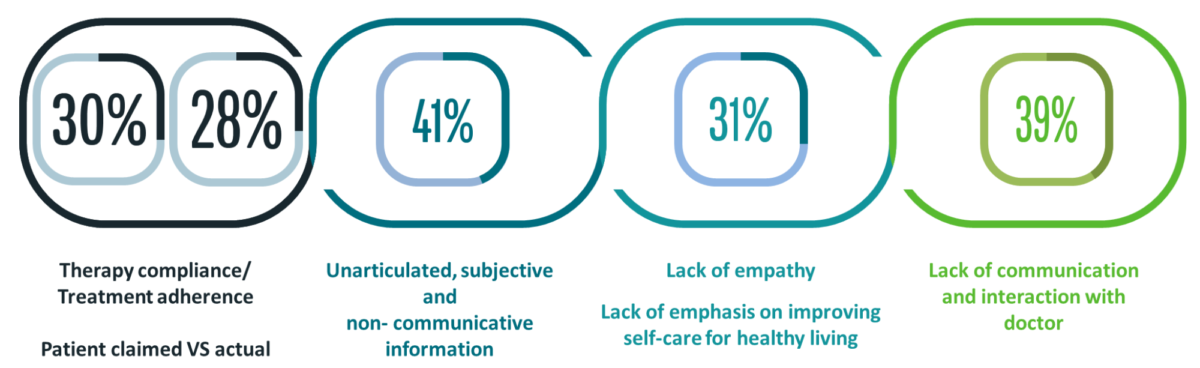
- Doctors in both countries stated that there’s a significant gap in what a patient claims vs. the reality. In particular, 30% and 28% of the doctors claimed compliance to therapy and treatment adherence by patients, respectively, were an issue.
- 41% of all doctors also claimed patients’ inability to articulate problems is an issue. This includes problems with expressing certain non-communicative information to doctors.
- Meanwhile, 31% of patients claimed ‘lack of empathy’ on the part of doctors.
- Lastly, 39% of the patients claimed ‘insufficient communication and interaction with doctors’.
All the above factors can be attributed to a common, broader communication gap between doctors and patients.
Resultantly, we wanted to understand how to close the patient/doctor communication gap. Closing this gap will benefit patients, doctors and the pharma, biotech, and other related industries. The next step was to conduct hybrid research, combining a quantitative survey and a qualitative tracked study, with the same control group and a test for 2 months. The aim was to map patient journeys in the USA and Brazil by employing new-age research methods on our deeply profiled healthcare respondents.
The goal was to conduct a patient journey study with two sample cells:
- A control group (400 patients/50 GPs): Patient data was gathered using conventional means
- A test group (80 patients/30 GPs): Patient data was gathered by using conventional means and supplemented with additional data from a smart wearable ‘glove’ worn by the patients. The smart device captured information such as blood volume pressure, heart rate, skin temperature and muscle tone, GPS data and general activity levels
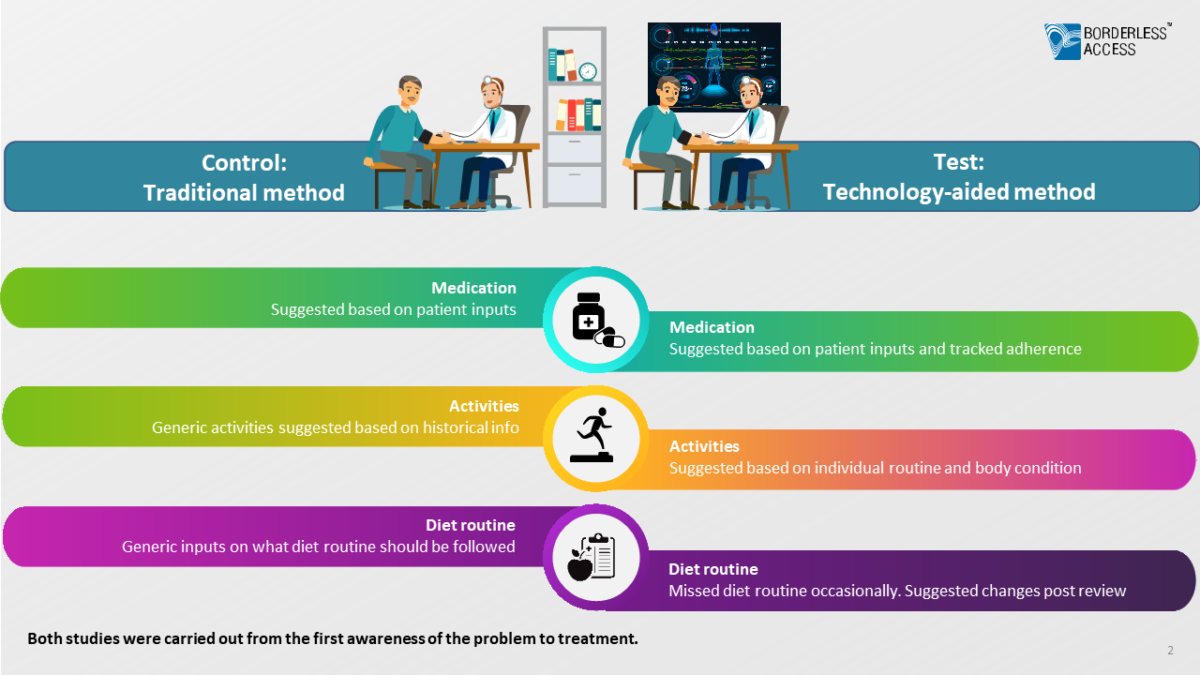
Both studies were carried out from the first awareness of the problems relating to diabetes to treatment.
The following observations were made:
Control group: Patient inputs to the doctor were minimum, limited by the doctor-patient disconnect as observed earlier. The treatment process was dependent on data monitored by doctors based on conventional treatment practices such as medical tests, patient inputs, and available historical data.
Also, doctor recommendations dependent on adherence to therapy and physical activity were dictated by available historical data and patient inputs.
The result was a conventional consultation where the treatment was significantly influenced by patient inputs alone.
Test group: In the second case, the doctors had access to data gathered from continuous monitoring of patients’ health and other parameters (not available for confidentiality purposes) through the smart device. This information helped fill the gaps in the information provided verbally by the patients. Information was further validated using passive data monitoring for precision diagnostics and the course of treatment, and medication was decided based on the comprehensive analysis of active and passive information.
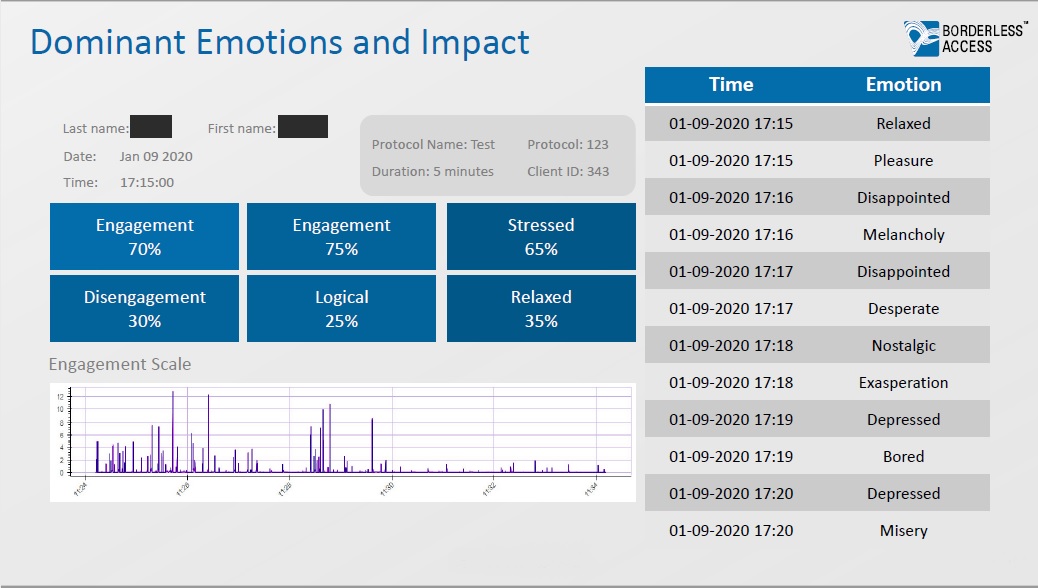
In the test group, doctor recommendations weren’t limited solely to patient inputs since the smart device allowed active tracking of patient activity, routine, and even certain aspects of therapy adherence. This made the recommendations more dynamic and suited to individual patient requirements.
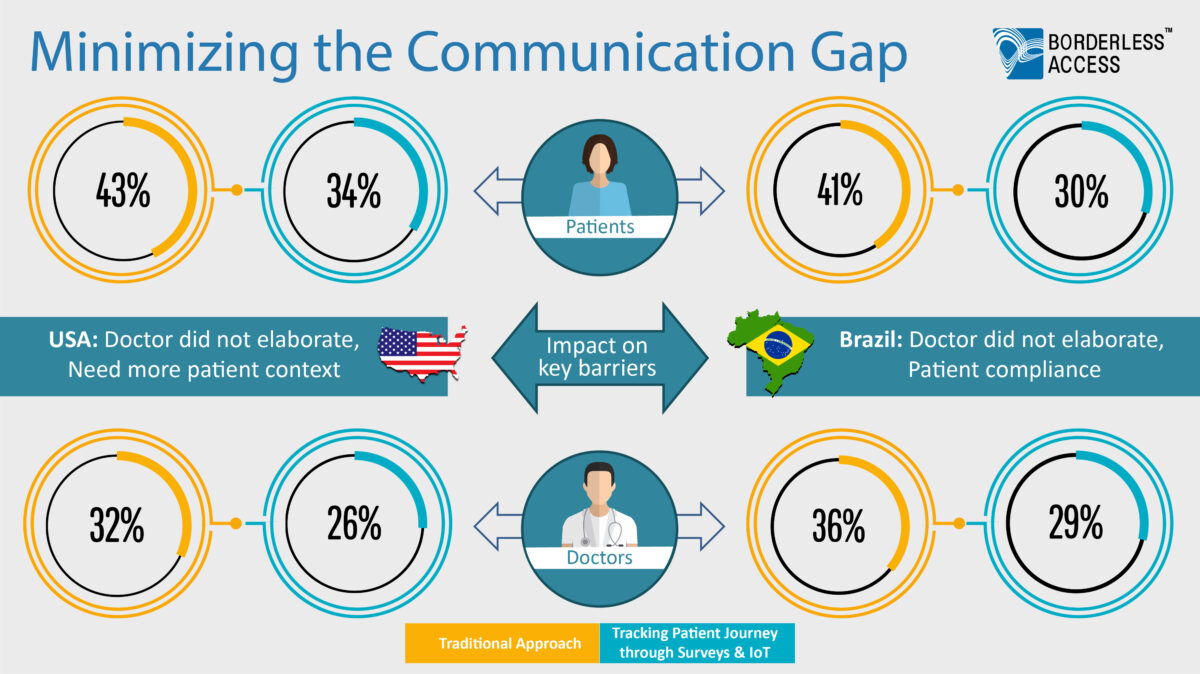
Source: PPES 2020 Post (Physician/Patient Experience Study) Borderless Access, n=400 patients and n=50 General Physician (Percentages shows are the top 2 box to the following question:
Q: On a scale of 1 to 7, how would you rate the overall ease and clarity of communication with your _______(Primary Physician/ Patients)
Upon completion of the study, a survey was once again conducted, which revealed that the doctor-patient communication gap in the test group had significantly reduced in both countries.
Conclusion
A digital, data-driven approach to healthcare market research can help healthcare professionals be more patient-centric. A forward-looking approach to patient-centric healthcare research involves three methods:
- The existing quality and quantity of patient information collected via smart devices will methodically change future feedback
- Tracking studies as a hybrid of technical and traditional surveys will become the new standard
- Passive data technologies are increasingly being used and the collected data will in the future be validated and analysed in new depth


