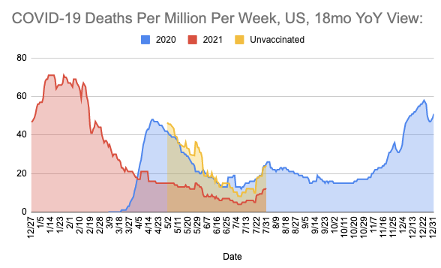
Last month, I published that we’d see another wave of cases and deaths, almost exclusively among the unvaccinated (Research World). To quote last month’s update, when “we factor into the model seasonality, based on last year’s deaths among unvaccinated, then the forecast increases to… 9,000 incremental deaths for the month of July, ending above 613,000 deaths at the end of the month.”
We ended the month within 1% of my model’s forecast (612,919 deaths).
My forecast was higher than COVID Forecasting Hub, which put incremental deaths at 7,794 and much higher than IHME, which projected 5,197 incremental deaths by the end of July. I think the difference between my model and the other models is I took last year’s patterns into account. I projected that those unvaccinated would continue to see the same rate of death from COVID as experienced this same time last year, while those vaccinated would largely be protected from deaths. That’s exactly what happened this last month.
CHART
While the estimate of deaths was accurate, the surge in cases was higher than expected.
In the US, cases increased from under 100,000 new cases per week at the end of June to about 550,000 in the last week of July. In Europe, Russia, France, Spain and Greece have cases surging. The UK and Netherlands showed a surge in June that appears to be abating now. Ukraine, Poland, Romania don’t show a surge in cases, but reporting in these countries has had a larger error margin in the past, so it is difficult to say with certainty their status. Generally, countries in the European Union have done a better job with reporting, and it currently appears some counties in the EU will see a 4th wave, but not all.
Something is different about this wave. Not only is the wave uneven across Europe and the US, the relationship between cases and deaths is changing due to vaccinations. While there is no formal reporting of vaccine breakthrough (VBTs) cases in the US, my analysis suggests VBTs make up a growing proportion of these new cases. The good news is that fully vaccinated people rarely die of COVID-19, and that is why I believe the Case Fatality Rate (CFR) is already falling — and will continue to fall.
CHART: Case Fatality Rate (CFR) 7-day Average, From July 1 to August 1, 2021
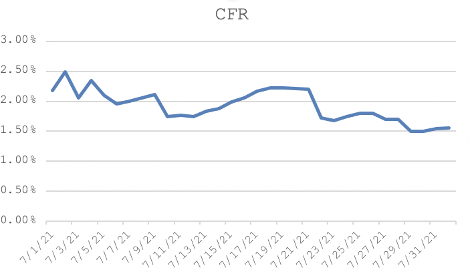
In the last 7 days of June, CFR was 2.1%, meaning about 1 in 48 people that tested positive for COVID-19 died. These were almost exclusively those unvaccinated. Today, in the last seven days, CFR is 1.5%, meaning 1 in 67 people testing positive died of COVID-19. I believe this is because more fully vaccinated people are testing positive for COVID-19. Since those fully vaccinated rarely die of COVID, it is changing the average CFR. I predict that rate will fall to about 1 in 100 (1%) by the end of August. Today, in the US, a little over half the total population is fully vaccinated. The European Union passed the US in the past month on “first dose”, and will likely pass the US on “second dose” later this month. Therefore, thanks to the protection afforded by the vaccine in the US and European Union, the CFR could fall even further as more people are vaccinated.
While vaccines are not providing as much protection from getting infected as we’d like, my research shows those vaccinated are significantly less likely to die, less likely to be hospitalized, recover faster and are less likely to infect others. All great benefits of vaccinations.
But “less likely” means some VBTs do infect others. Some, particularly those over 60 do end up in hospital. And some, particularly those over 70 do die of COVID-19. That’s why we will see more precautions, like masking, put back in place.
Three month forecast:
The three month forecast (made at the end of April) projected the US would end July with 613,923. We ended with 612,919, within 3% of the forecast based on the incremental deaths. But, during July, Delta went from a relatively small minority of cases in the US and Europe to the dominant strain. Delta is more infectious, and deadly, based on my analysis. Therefore, the three month forecasts I made in May and June will be too low because Delta changed the trajectory.
Back in November, I would have expected the level of vaccination in Europe and the US combined with recoveries from infection to exert enough downward pressure on the virus to effectively end the pandemic in Q3. However, there are stubborn pockets of unvaccinated people that are dying at the same rate as this time last year — and, because of the J&J pause, vaccination rates slowed such that the US is 15% behind my November 2020 projection. At the same time, the Delta is much more infectious. In combination, we are experiencing a fourth wave in the US and Europe.
My current data for July shows only a modest downward pressure on incremental COVID-19 deaths from vaccination and natural recovery (cumulative immunity). For this reason, we do not believe we will achieve so-called “herd immunity” in the next 60 days. Instead, we are likely to contend with a Fall and Winter surge. With a return to in-person school beginning in less than a month, our analysis suggests that mask wearing and vaccinations among those under 12 would be beneficial.
Because those under 12 are not eligible yet to be vaccinated, we expected to see the ratio of infections among 0-19 to increase, similar to the pattern observed in our analysis of data from Israel, where most of the infections today are among youth. In the US, examining HIS data set through July 11, as expected, the rate picks up in April from less than 15% to over 30%. But then, in late May, the rate drops off again, back to around 15%. (The red line is the 14-day moving average).
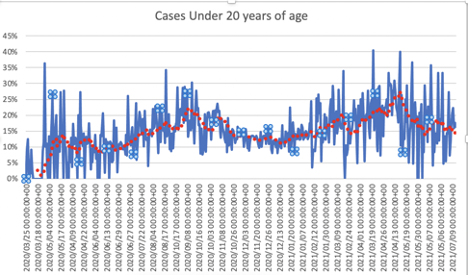
An explanation for this pattern is that in-person school increases the rate of infections among our youth. And, when school sessions ended for summer break, rates of infection decreased as a result. If this explanation is correct, it means in-person school this fall could increase infections and breakthrough cases.
While youth rarely die of COVID, they can be a reservoir of infections and can spread it to others who are at greater risk of hospitalization and death. To date, over 47,000 children, 0 to 17 have lost a parent to COVID-19. While the risk of death from COVID for a child is low, it is not zero. Children can die, or require hospitalization, or suffer longer-term damage from COVID-19. The Delta variant may increase these negative outcomes. At the same time, there is value to in-person school for both the child and to working parents. Polls show the majority of parents want in-person school for a variety of reasons.
In light of this data, how do we make in-person school work?
First, expect regulatory bodies to approve vaccinations for those under 12 years of age. Second, expect masks and other precautions to be implemented in an effort to return kids to the classroom as safely as possible. In areas with high cumulative immunity due to high vaccination rates or natural recoveries, it may be that there is adequate protection to safely return to school. In areas with less cumulative immunity, schools may be a source of additional outbreaks.
In sum, my model expects a fall/winter wave, but it will be almost exclusively among the adults not vaccinated.
Because of Delta, my 3-month forecast has increased significantly. With a starting point of 612,919 reported deaths as of the end of July due to COVID-19 in the US, the most conservative scenario is projecting 681,268 deaths versus 629,966 at the end of October in the Pre-Delta projections. This scenario assumes those unvaccinated see the surge in deaths, and change their behaviors by the end of August. Since deaths lag by about three weeks, the wave will end in the back half of September. On an incremental basis, which is what I use to calculate model accuracy, the forecast quadruples over the pre-Delta forecast.
The worst case scenario considers that those un-vaccinated do not change their behavior at all. Due to misinformation, some unvaccinated do not believe the death toll statistics, and have little to no intention of changing their behaviors vis-a-vis COVID. Instead of seeing a decline in case growth and deaths to end the Fourth Wave, the US experiences one big wave that carries through to the end of the year. In this scenario, we barrel to herd immunity in the US the hard way — with an incremental 168,000 deaths between now and the end of the year (about 100,000 between start of August and end of October). This scenario equates to more than three quarters of a million hospitalized. Hospitals in areas with low vaccination rates will be most impacted.
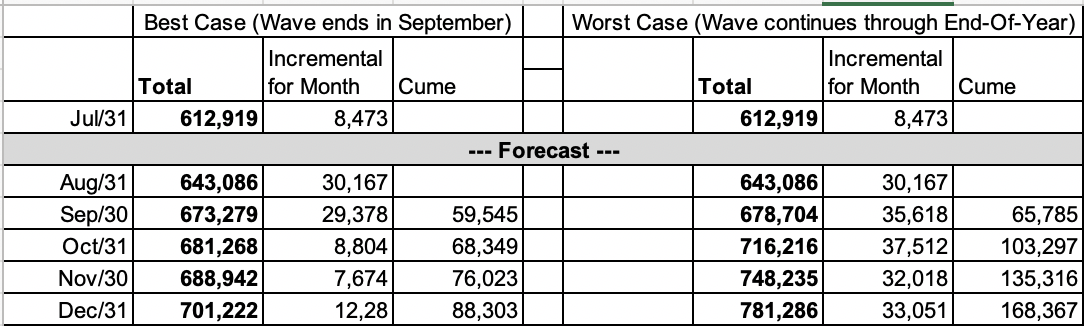
Note: The Worst Case Scenario will now be reflected in the www.speakerrex.com/dash.html dashboard view. This scenario is labeled Briggs-3.1 (Delta), given the significant revision over the Briggs-3 version from Nov-2020.
Dollars don’t fully capture the toll on families, communities or the qualitative experience of the economy and everyday life. With that caveat, consider the average cost of COVID hospitalizations at $73,000 each (source: FairHealth.org). As hospitalizations average at least five times the death toll, in the worst scenario, the hospital tab is over $61.5 Billion. With a statistical value of a life of $8.7million in the US, the total cost of lives lost over the next six month plus hospitalization costs in the worst case scenario is $1.5 Trillion. That compares to a cost to completely vaccinate every remaining unvaccinated adult in the US of $19 billion ($30 cost per dose + $40 cost to administer dose x 2 doses x 138 million adults unvaccinated).
While the stress will be felt by all the medical frontline workers, and the effects will ripple through the US Service economy, it will be the unvaccinated that suffer the most. They will account for the majority of all deaths and hospitalizations. I estimate about half the un-vaccinated population has already had COVID-19 and likely has some level of protection. Therefore, I expect the deaths per million per week among the unvaccinated to be about a third lower than the peak from last year. A variant that causes reinfections at a high rate could change this projection substantially.
While those fully vaccinated will be largely protected from death due to COVID, the exception will be those over 70. In the study I worked on with Brown, Harvard, Nevada Public Health Lab, and Washoe County Health District (recently submitted to CDC for publication), we found great protection from the vaccine, but those over 70 had risk of a breakthrough infection that could land them in the hospital, and in a few cases, result in a COVID-19 death.
Some believe Delta will lead to herd immunity faster, because it is so infectious, and prior infection confers a level of immunity to future infections. But more infectious also means a higher threshold for herd immunity. Prior to Delta, I calculated the threshold to be around 85%. If Delta increases the threshold into the 90% range, then in either the best or worst case scenario, the US will not reach herd immunity until early 2022.
As of today, there is only a weak correlation (r2=.33) between cumulative immunity and the rate of increase in deaths. Instead, deaths predict future vaccinations in a classic case of reverse causality. I am working on implementing a tracking mechanism for the US and Europe so we can see when vaccinations and prior infections do indeed predict a slowing of cases and deaths as that will signal we are very close to herd immunity.
In addition to the risk that those unvaccinated will not get vaccinated, mask up or social distance in significant numbers to end the Fourth Wave, the greatest risk we face is re-infection. If the virus mutates such that those who have recovered no longer have immunity, then that will be a significant set-back.
The US and European Union should expect boosters for 65+ and potentially a re-evaluation of the interval between first and second doses. This will lower deaths in the US and the European Union, but it will have knock-on ramifications to the rest of the world, whose supply of vaccines was already less than desirable. Better protecting our elderly will mean many countries will have inadequate protection from COVID-19 this winter, when another wave of infections could increase the destruction to lives and livelihoods. Ukraine, Bosnia Herzegovina, Belarus, Bulgaria — these are some of Europe’s least vaccinated countries. African countries are the furthest behind on vaccinations. In many cases, it’s not for want of the vaccine, but rather for lack of supply.
I’d like to end this month’s update on a bright note. But, Delta has taken the wind out of my sails. I was enjoying that briefest of summers, when I was at the beach with my extended family and sharing a laugh and seeing their smiling faces. But, that moment has passed, I am grateful for it. I recognize how fortunate I am. Now, I put my mask back on, and return to my work with the Ad Council to aid in the vaccination effort. There is a path forward to more moments with family and friends, probably in early 2022, when we’ve succeeded at getting more than 70 percent of our population fully vaccinated and figured out a way to get more vaccines to the people and countries around the world that want them.


